A comprehensive study was conducted between 2012 and 2018 in 15 community hospitals in the United States with the aim of improving the quality of blood transfusions in patients. An anonymous review of patient records who received blood components was done in a retrospective review process. Each hospital had a qualified transfusion director and met accreditation supervision requirements for blood review.
Although the hospitals had described their use of blood as “good,” only three of them had evidence–based blood management programs (#PBM). Hemoglobin values below 7 were used to justify red cell transfusions, while several employed proactive detection and intermittent deriving to the medical director. However, only one hospital provided documentation that supported active intervention in blood use. Although transfusions were in line with appropriate laboratory guidelines, none of the hospitals provided documentation that supported good patient blood management or anticipated the level of unnecessary blood use found in the study.
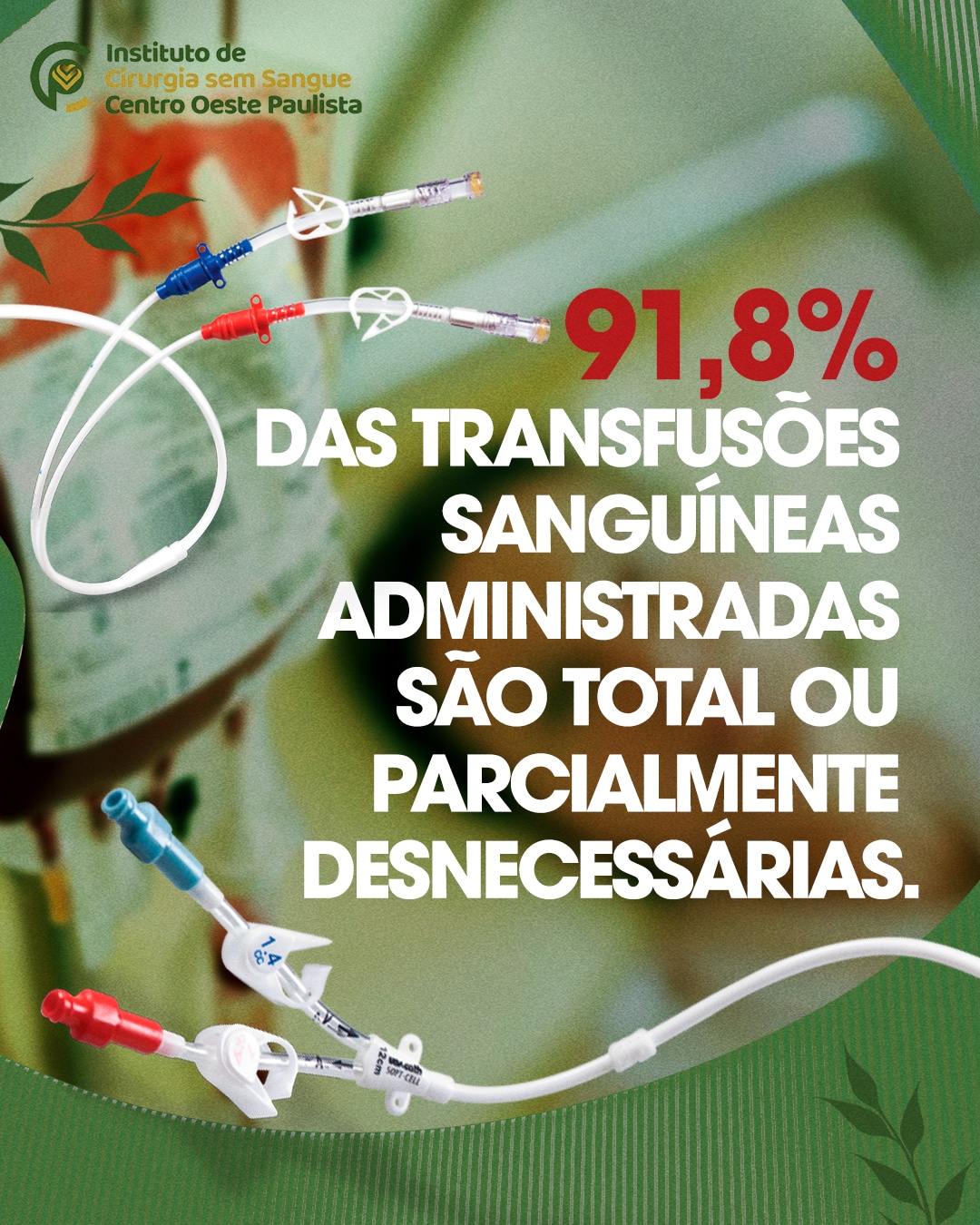
The results indicated that patients on average received 4.3 units of blood, with only 8.2% receiving unneeded units. Over half of the patients (55%) could have been managed without at least one type of component, while 44.6% could have been managed entirely without transfusion. Furthermore, between 2,713 and 3,306 units of blood were likely unnecessary, resulting in an increase of 0.38 days of hospital stay per one of those unnecessary units.
Before the review, none of the hospitals had recognized the substantial, unnecessary use of blood at their institution. Unnecessary use of blood was attributed to overreliance on laboratory transfusion criteria and lack of blood monitoring, which resulted in potential patient harm and avoidable cost.
Information sourced from: https://tinyurl.com/a985pf2d